- Critical Care Services
- Introduction to Critical Care
- General Information

We have 33 general critical care beds (Level 2&3) divided between Unit 2, Unit 3 and General Critical Care Unit. We also have input into the Spinal High Dependency Unit (L2 x 5 beds) and the Neurosurgical High Dependency Unit (L2 x 8 beds). There is a separate Cardiac Intensive Care Unit and Paediatric Critical Care Unit.
We take referrals from any area of the hospital. In your role within the critical care team you may be asked to provide care for a patient in any of these areas.


We have 9 ACCP’S who are from senior nursing or physiotherapy backgrounds. They have completed an additional 3- year training programme to work as part of the resident doctor rota. There are 2 more in training. They are professionally regulated through NMC/ACPC and FICM. Their role is almost identical to that of a junior doctor and includes patient assessment and management, practical procedures, drug prescription, requesting investigations and verification of expected death. They know the clinical area well and are a useful source of support to new colleagues
We have more than 200 members of nursing staff, a physiotherapy team led by Andrea Henderson, occupational therapists Sharon Barker and Charlotte Jordan, critical care pharmacy team led by Luke Alderson and dietetics team led by Rachel Edson.


We have a 24/7 Critical Care Outreach team at The James Cook University Hospital which will follow up all discharges from critical are and review referrals.
The team plays a vital role in monitoring and assessing acutely unwell patients anywhere in the hospital and assisting with any interventions that may be required prior to patients being admitted to a critical care bed.
We are aware that every doctor has a different level of prior experience and knowledge. We do not expect you to always know what to do but you should always ask if you are unsure.
There are always plenty of people around during the daytime – middle grades, very experienced staff grades and consultants. Out of hours the ICU middle grade should be contacted on bleep 1005. If no-one is available or further advice is needed the 3rd call anaesthetist should be called on bleep 4598.
The unit is covered 24 hours a day, 7 days a week by a Consultant in Intensive Care.
If you are UNSURE what to do, or about instructions you have been given, please ASK.
We hope you will learn lots, develop your clinical skills and most of all enjoy working with us.
Day to day work on the units
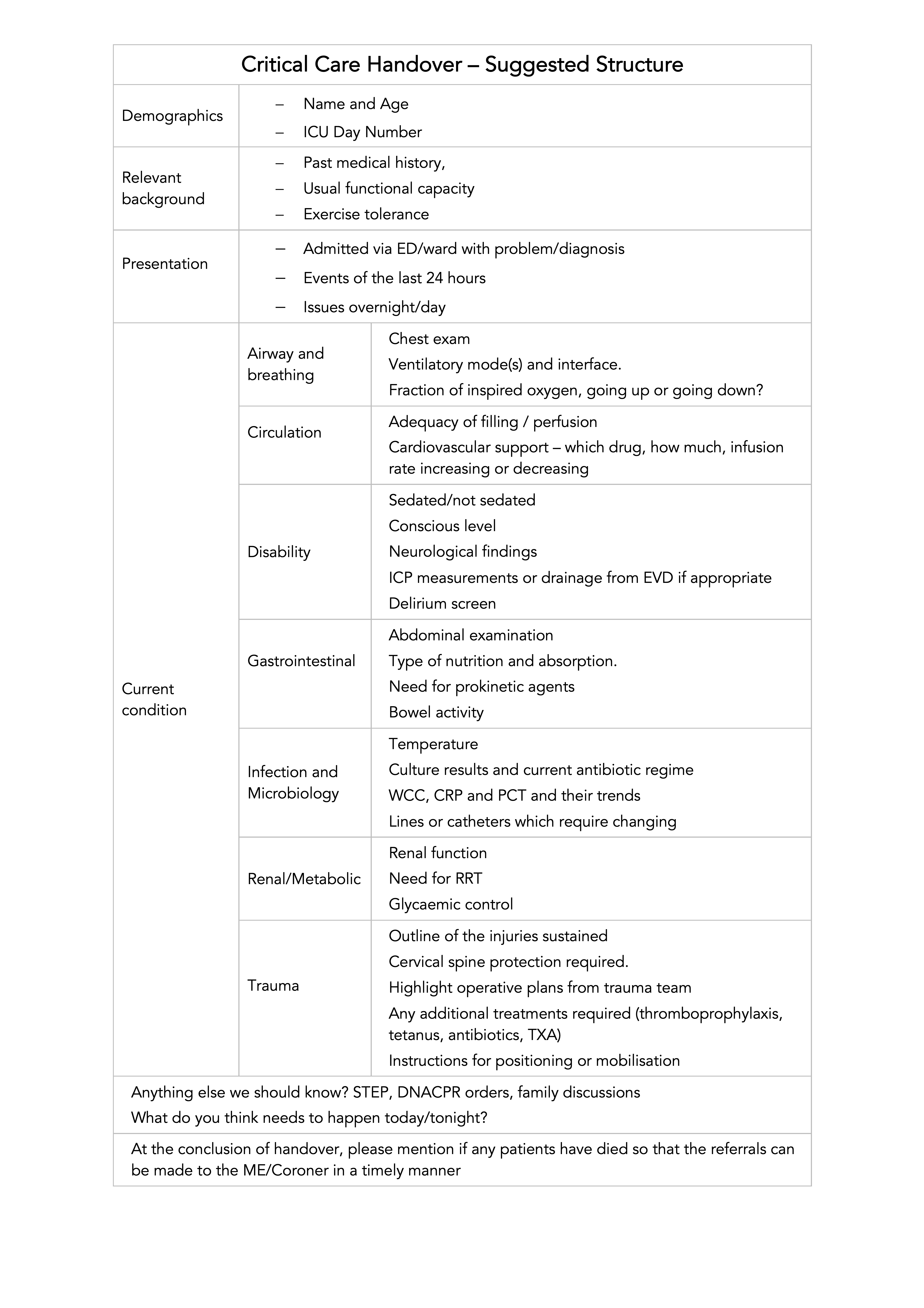
A daily handover from night shift resident and middle grade to daytime staff, resident, middle grade, ACCP and Consultant, occurs between 8.30 – 9.00hrs.
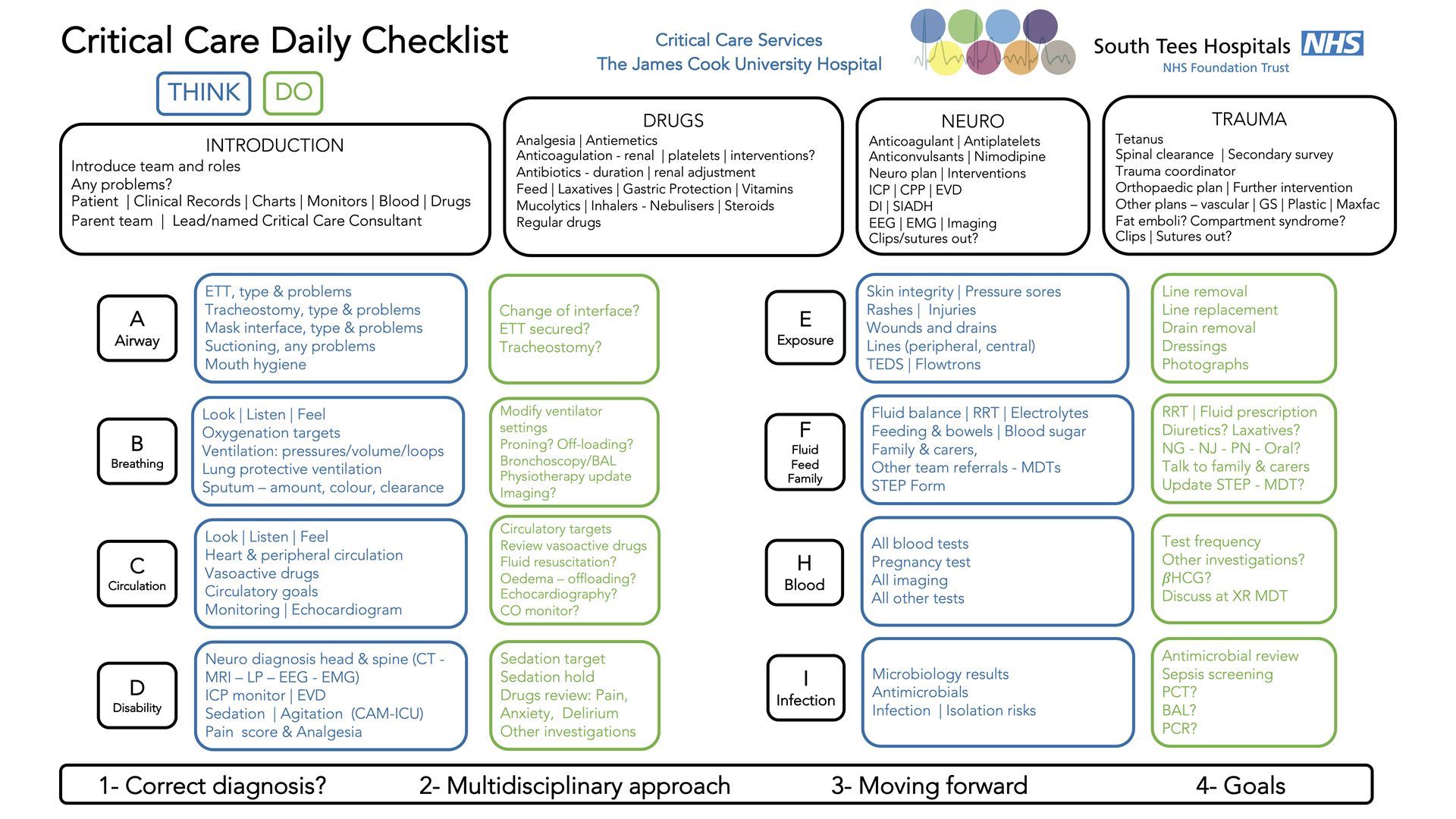
The ward round will then proceed to review each patient and make a plan for the day. Patients who are immunosuppressed should be seen first and those with contagious infections should be reviewed at the end of the round. A list of tasks for each patient will be generated. We encourage the use of the ward round jobs folder (available on each unit) rather than keeping your own list - this ensures that everyone is aware of all tasks and work is not duplicated or omitted. Tasks should be prioritised to ensure smooth running of the unit.
On Monday, Wednesday and Friday afternoons, a microbiology round occurs on ICU with the Consultant Microbiologist. Please ensure all microbiology information is documented in the notes and drug chart and passed on at handover.
We have introduced a standardised ‘panel’ of Web ice blood test requests for ICU admissions, basic daily set (stable patients) and extended daily set (unstable patients), any additional individual tests can be added as needed. These can be found in the collections menu (ICU collections) on Web ice requests. See Appendix 1 at the end of the document.
The night shift handover occurs between 20.30 to 21.00hrs. Night shifts can be very variable. If the night shift is quiet this is an opportunity to ensure that all x-rays and results are reviewed / chased up, all documentation is up to date etc. You should ensure that you know each patients history and progress thoroughly for the morning handover.
The focus on the morning ward rounds should be to see the sick patients first followed by the patients highlighted for discharge. There will be a later surge in activity as the elective admissions arrive from theatre. This can often occur in the late evening.
Rota
The rota is published on a rota software called FINDMYSHIFT. You can access it on a web browser or an app on your smartphone. You will be given a login when you rotate with us. The ICU secretaries and Dr Hyde are in charge of theTier 1& 2 rota. Please see rota guidelines and email about any rota issues to:
stees.criticalcarerota@nhs.net
There is usually a resident doctor or ACCP in each ICU and 2 on GCC with a middle grade on each unit and 4 Consultants during the daytime. At night there is 1 resident on each unit, 2 middle grade to cover all 3 units and a Consultant on-call.
Sickness
Please contact the ICU office as soon as you recognise that you will be too ill to work and email stees.criticalcarerota@nhs.net.
If this is out of office hours please contact the on-call Consultant. You should also inform the person who holds your sickness record card. If you are sick for longer than 7 days you will require a sick note from your Doctor.

Uniforms
You should wear a clean uniform for each shift and change if it becomes visibly soiled. Scrub suits are available should you wish to wear them. They can be purchased from Anne, Clare or Jade and cost £15 per set. They are then yours to keep. If you choose not to wear a scrub suit the trust uniform policy must be complied with – see below.
The trust operates a bare below the elbow policy.
ALL staff in any clinical area are expected to adhere to this. All jewellery apart from plain wedding bands should be removed.
Uniforms and work wear when providing patient care |
|
GOOD PRACTICE |
WHY |
|
Dress in a manner which is likely to inspire public confidence |
People may use general appearance as a proxy measure of competence |
|
Wearing short sleeved shirts and blouses Avoid wearing white coats |
Cuffs become heavily contaminated and more likely to come into contact with patients |
|
Change into and out of uniform at work |
Patients confidence in NHS may be undermined |
|
Wear clear identifiers ( Name badge) |
Patients wish to know who is caring for them |
|
Change immediately if uniform or clothes become visibly soiled or contaminated |
Visible soiling might be an infection risk and is likely to affect patient confidence |
|
Tie hair back off the collar |
Patients prefer to be treated by nurses/ midwives with short or tidy hair and a neat appearance |
|
Keep finger nails short and clean |
Long and or dirty nails can present a poor appearance and long nails are harder to keep clean |
|
Change into a clean uniform at the start of each shift |
Maintains professional appearance |
|
Wear soft-soled, closed toe shoes |
Closed toe shoes offer protection against spills. Soft soles reduce noise, which can disturb patients rest |
BAD PRACTICE |
WHY |
|
Wearing uniform to go shopping or similar activities in public |
Patients confidence in the NHS may be undermined |
|
Wearing false nails for direct patient care |
False nails harbour micro-organisms and can reduce compliance with hand hygiene |
|
Wear hand or wrist jewellery/wristwatch (a plain wedding ring may be acceptable) |
Hand/wrist jewellery can harbour micro-organisms and can reduce compliance with hand hygiene |
|
Wearing numerous badges or other adornments |
One or two badges may be acceptable, too many looks unprofessional and may cause injury when moving patients |
|
Wear neck ties ( other than bow-ties) in any care activity which involves patient contact |
Ties are rarely laundered but worn daily. They have been shown to be colonized by pathogens |
|
Carry pens/scissors etc in outside breast pockets |
May cause injury when moving patients. |
|
Wearing uniform sloppily e.g. wearing cardigans when providing direct patient care or wearing uniform dress without tights/stockings |
Patients expect staff to have a neat appearance. |
|
Wearing excessive jewellery, including necklaces, visible piercing and multiple earrings. Where earrings are worn, they should be plain studs. |
Excessive jewellery looks unprofessional and may be hazardous |
DoH, Uniforms and Workwear. An evidence base for developing local policy, September 2007
MDT meetings
We hold multi-disciplinary meetings to discuss the needs of long stay patients. You are welcome and encouraged to attend these meetings.
Morbidity and Mortality Meetings
We hold monthly M&M meetings to review some of the patients who have died on our units and discuss any incidents or morbidity issues.
Meetings are held between 1-2pm on the first Wednesday, Thursday or Friday of the month .
Everyone is welcome to attend. They are a valuable learning tool.
If you wish to participate in the meetings by presenting a case please contact the consultant chairing the meeting.
Patient diaries

Patient diaries are a useful way for patients to understand what has happened to them during their critical illness.
It is a written (sometimes photographic) contemporaneous record of their critical care stay that they can take away with them.
All members of the multi-disciplinary team are encouraged to participate on the patients’ behalf. Please discuss with a senior member of the Medical or Nursing team.
Patients have asked in several ocassions at the ICU follow up clinic for doctors to write on the diaries.
Catering facilities
The coffee room on the critical care units is always fully stocked with tea, coffee, milk, cold water, squash, bread (with toaster), butter and a selection of jams / spreads. £5 per month should be paid to the secretaries.
There are two large fridges to store any packed lunch and two microwaves for all staff use. Please label your food with your name and the date on the stickers provided. Any unlabelled food will be thrown away.
Please keep the coffee room clean and tidy at all times.
There are a variety of food suppliers within the main hospital: canteen, WRVS, Costa, Marks and Spencer and WH Smiths.
After 10pm there are NO catering facilities within the hospital. There is a trolley service to each ward. This usually arrives at ICU around 10.30pm.
Rest and general wellbeing
There is a Junior Doctor’s office on the main ICU corridor for the use by all junior medical staff. It contains a bed to allow you to get some rest if your shift is quiet. There are also en-suite bathroom facilities. It is for use by all members of the junior medical team so please try to keep it tidy.
It is essential that you have adequate time for meal breaks. Because much of work is emergency driven it is difficult to predict timing of breaks. It is essential that you work as a team to ensure that everyone has the opportunity to eat/drink with safe provision of clinical cover.
If you feel too tired to drive at the end of your shift, it is really important that you take rest before you attempt to drive. The residents’ room should be available. Feel free to put a note on the door requesting not to be disturbed. If you are struggling to find a place to rest, please seek help from the duty consultant.
If you need a break off the unit, please let inform the sister in charge of your contact details before you leave.