-
Introduction
The aim in the management of traumatic brain injury is to avoid and minimise secondary brain injury. Primary brain injury occurs at the time of the injury. High quality care is essential to prevent secondary brain injury.
- Maintaining an adequate Cerebral Perfusion Pressure along with adequate oxygenation is central to the prevention of secondary injury.
- Cerebral perfusion pressure (CPP) = Mean arterial pressure (MAP) – intracranial pressure (ICP).
- Secondary brain injury may therefore occur as an increase in ICP and/or a decrease in blood pressure
Raised ICP is associated with:
- Low PaO2 and/or High PaCO2
- Increased cerebral oxygen consumption (fitting, pyrexia, hyperglycaemia)
- Obstruction to venous drainage (head position, coughing, tube ties)
- Cerebral oedema (typically peaks in injured brain cells at 72hrs)
- Expanding intracerebral, subdural or extradural haematoma.
- Hydrocephalus (outflow obstruction in traumatic SAH)
If the ICP is elevated (Normal ICP is 0-10 mmHg, ICP > 20 mmHg for more than 5 mins is abnormal), cerebral blood flow may be compromised even with a normal blood pressure. A single, short period of hypotension (MAP < 70mmHg) is associated with a worse outcome.
Cerebral perfusion is autoregulated in health to maintain constant cerebral blood flow within a wide range of blood pressure. In brain injury (e.g. trauma, infection, bleeding) this autoregulation may be lost. When this happens, hypertension may conversely lead to an increase in intracranial blood volume in normal brain, and an increased ICP and reduced perfusion of the injured brain.
The aim is to avoid hypo/hypertension prior to ICP monitoring and then to optimise ICP and MAP to achieve a satisfactory CPP (see CPP & ICP guidelines below).
PaO2 and PaCO2 also affect cerebral blood flow. Cerebral blood vessels dilate with increasing PaCO2 or decreasing PaO2which leads to an increase in intracranial blood volume, increased intracranial pressure and reduced cerebral perfusion pressure. Cerebral blood vessels vasoconstrict with decreasing PaCO2, which will reduce intracranial volume. Unfortunately, cerebral vasoconstriction will reduce cerebral perfusion unless blood pressure is increased.
The aim is to avoid/minimise hypocapnia, hypercapnia and hypoxia.
Initial management of Traumatic Brain Injury
- ABCDE assessment and management
- CT scan if stable and no life-threatening injury requiring immediate surgery
- Discuss with neurosurgeons:
- Theatre, e.g., evacuation of haematoma, etc.
- Critical Care: ICP monitoring
-
ABCDE assessment and management
Airway
The first priority must always be to secure, maintain and protect the airway.
Cervical spine injury should be assumed to be present.
Indications for intubation and ventilation after head injury:
- Immediately:
- Coma (not obeying, speaking or eye opening), i.e., GCS <9
- Loss of protective laryngeal reflexes (pooling secretions/no swallowing)
- Hypoxaemia (PaO2 ≤ 13 kPa on oxygen 15 l/min and reservoir bag)
- Hypercarbia (PaCO2 ≥ 6 kPa)
- Spontaneous hyperventilation (PaCO2 < 4.0 kPa)
- Respiratory arrhythmia
Before transferring out of ED (to CT/theatre/ICU:
- Deteriorating or fluctuating consciousness (drop on GCS ≥ 2 points)
- Drop in motor score ≥ 1 point
- Bilateral fractured mandible or difficulty with airway maintenance
- Copious bleeding into mouth
- Seizures
Breathing
Assess adequacy of ventilation clinically and by arterial blood gas analysis. Aim for PaO2 11-13kPa (higher than normal ICU patient in order to increase brain tissue oxygenation and reduce chance of unintentional hypoxaemia), PaCO2 4.5 – 5.0 kPa. Avoid hypocapnia (PaCO2 < 4.0 kPa). Note: EtCO2 will be approx. 0.7 kPa lower than arterial (if the blood pressure is normal and in the absence of significant lung pathology).
Circulation
If GCS < 8, assume elevated ICP (20-30 mmHg) and maintain MAP 80-90 mmHg to ensure CPP 60-70 mmHg. If euvolaemic, use vasopressors/inotropes (noradrenaline or ephedrine 3mg boluses) to maintain MAP if needed (caution required in elderly or those with heart disease).
An isolated head injury is rarely the cause of shock, especially in adults. Look for signs of hypovolaemia, (tachycardia, pulse pressure variation with respiration/ventilation, capillary refill, oliguria). Actively look for a source of bleeding (multiple fractures, thoracic, abdominal, pelvic haemorrhage) and consider general surgical input. A patient in persistent shock despite fluid resuscitation must not be transported to CT or critical care until the source has been identified and controlled as part of the resuscitation.
Use 0.9% sodium chloride initially, or blood/FFP as required to correct coagulopathy. Avoid hypotonic fluids (Hartmann’s or dextrose solutions) and albumin (SAFE trial).
If persistent hypotension despite adequate filling (clinical or echo assessment), consider myocardial contusion, tamponade, pneumothorax, high spinal cord injury, coning.
Catheterise the bladder and measure urine output.
ICU Management
Initial stabilisation in critical care
Ventilation
PaO2 11-13kPa, PaCO2 4.5-5.0kPa
VT 6-8ml/kg, f 12, I:E ratio 1:1.5-1:2, PEEP 5-10cmH2O
Sedation
Propofol 2-4mg/kg/hr; Alfentanil 10-50mcg/kg/hr titrated to effect
Atracurium bolus/infusion if indicated
Circulation
CPP 60-70mmHg (MAP 80-90mmHg until ICP bolt)
Monitoring
A-line, CVP, ECG, temp, end tidal CO2
Investigations
ABGs, U&E, FBC, Coagulation screen, G+S
Reassess ventilation
- Initial VT 6-8ml/kg
- Ideally use a volume control mode to ensure consistent minute ventilation (e.g. SIMV) to regulate PaCO2 or use BIPAP with close volume/EtCO2 alarm limits
- If plateau/peak pressure is high, consider reduction in tidal volume or BIPAP
- If BIPAP is used, set alarm limits for minute volume close to desired target to detect varying minute volume due to changes in compliance.
- Monitor ETCO2 (with alarm limits set to maintain desired range)
- Use rate to control PaCO2
-
Use FiO2 /PEEP to control PaO2. A minimum of 5 cmH2O PEEP should be used to reduce atelectasis as for any other ICU patient. Up to 12 cmH2O PEEP can be used in head injured patients with minimal effect on ICP, providing that the patient is euvolaemic and does not have markedly reduced lung compliance (transmission of increased intrathoracic pressure to brain).
If PaO2 < 11 kPa despite FiO2 > 0.5 and PEEP 12 cmH2O discuss with consultant after appropriate assessment. Careful proning may be preferable to APRV and sustained PHigh.
Reassess circulation
- Aim for CPP 60-70mmHg, maintain MAP 90 mmHg until ICP monitor inserted
- Is the patient adequately filled? Assess clinically and/or with Echo/Cardiac output monitoring.
- Rule out ongoing haemorrhage - Consider chest, abdomen, pelvis, long bone fractures
- Seek orthopaedic or general surgical advice
- Inotropic support as indicated
- ICP monitoring
-
All patients with GCS < 8 and traumatic brain injury should have an ICP bolt inserted by the neurosurgeons unless the injury is so severe that active management is considered futile or the CT appearance does not correlate with the clinical picture (e.g. suspicion of seizure activity/alcohol/drugs affecting GCS).
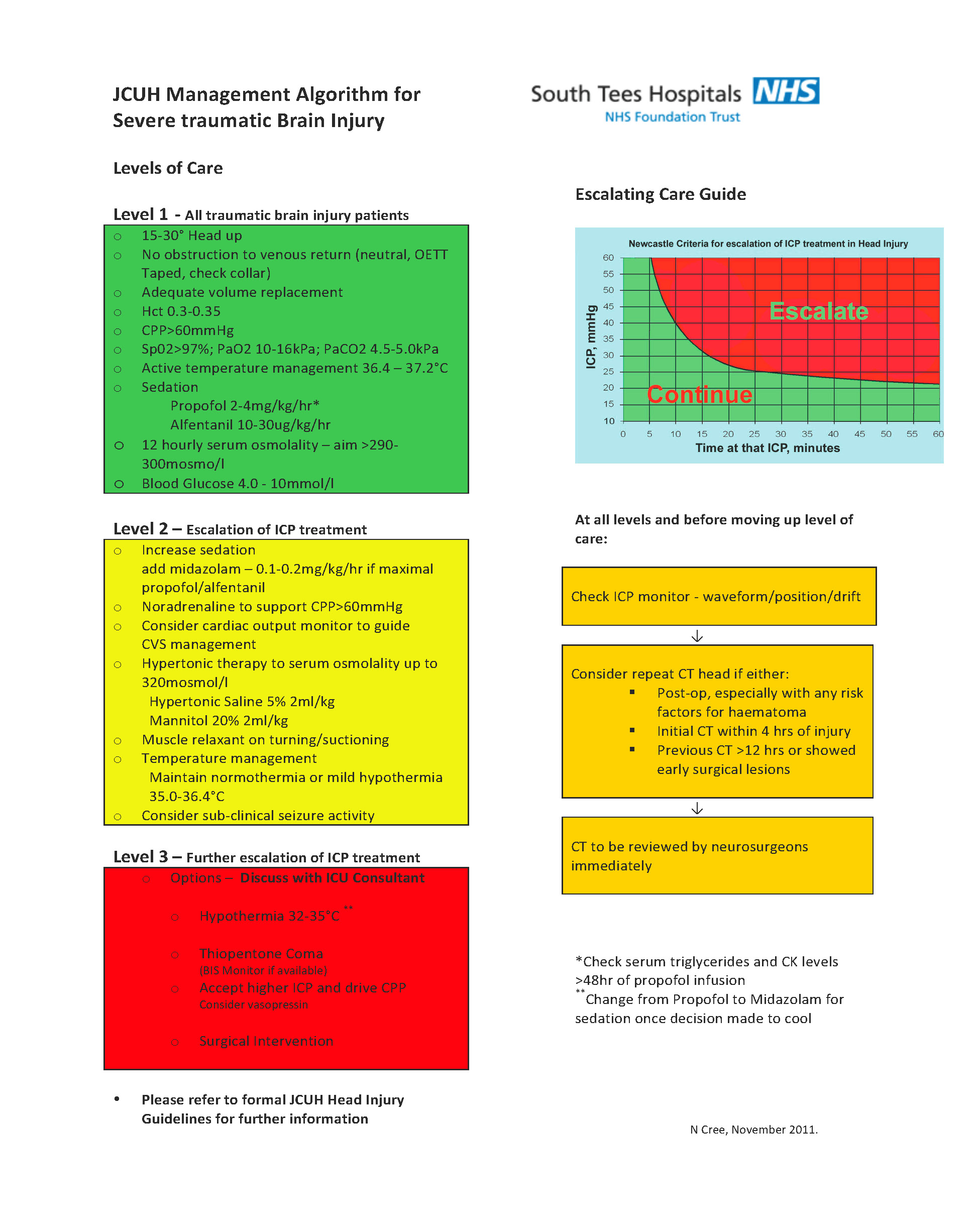
If ICP > 20mmHg see ICP guidelines
Sedation
Avoid coughing and straining. Ensure adequate sedation prior to intervention (e.g. suctioning) and avoid clustering activities together
Propofol & Alfentanil
Start initially with propofol 2-4mg/kg/hr and alfentanil 10-30mcg/kg/hr.
Reduce the dose in hypothermic patients (1-3mg/kg/hr) to avoid propofol infusion syndrome.Midazolam
Midazolam 0.1-0.2mg/kg/hr may be added to propofol if sedation is inadequate at maximum dosesClonidine
0.5-2mcg/kg/hr may be added to sedation when weaning in hypertensive patients.Remifentanil
Remifentanil can be used short term when weaning towards extubation (See separate guidelines).
-
Positioning
- Head up 30 degrees
- Neutral head position
- No obstruction to venous return (e.g. ties/collar)
- Spinal clearance (see separate guidelines) at earliest opportunity: Tape and sandbags with bed flat and head up tilt (C-collar for log roll/transfer only)
-
Osmolality
- Aim 300-320 mOsmol/L if raised ICP.
- Aim for Na 145-150 mmol/L (alternate 0.9% saline and 1.26% NaHCO3 to avoid hyperchloraemic acidosis)
- If ICP raised, aiming for Na 150-155 mmol/L may be appropriate.
- Avoid hypotonic fluid (Hartmann’s, 0.18% NaCl/5% Glucose etc)
- Check U&Es and Osmolality every 12hrs initially and 2hrs after giving Mannitol or Hypertonic saline.
-
Glucose
Normal ICU glycaemic control: blood sugar 6.0 – 10.0
-
GI tract
- Enteral feed immediately.
- Gastric protection as per unit protocol
- Routine ICU laxative protocol
-
Temperature
- Avoid hyperthermia: cool if needed, to maintain temperature 36°C (this ensures temperature does not go above 37°C)
- DO NOT use Prophylactic Hypothermia (POLAR – Glasgow Outcome Score Extended at 6 months identical and higher pneumonia and ventilator days in hypothermia group.
- Consider Therapeutic Hypothermia (34-36°C) for refractory high ICP – (Eurotherm-3235 suggested higher mortality and worse Outcome Scores in hypothermia group but other studies suggest benefit in refractory high ICP)
- Seizures
- Consider prophylaxis in high risk patients (e.g., known epilepsy/temporal lobe damage/depressed skull fracture)
- Only use within first 7 days of injury (unless treating seizures)
- Load with Phenytoin 18mg/kg iv (at <50mg/kg/min) then 100mg iv TDS for 7 days
- Or Levetiracetam 1g iv then 1g BD iv for 7 days
-
LMWH
- Discuss with surgeons
- Consider LMWH DVT prophylaxis after 72hrs depending on pathology. All patients should have mechanical calf compression from admission- Primary brain injury may cause hypercoagulability and with immobilisation VTE risk is increased (25% incidence even with calf compression). Age, subarachnoid blood and other injuries further increase risk.
- Low dose anticoagulation has the potential to cause significant intracranial haemorrhage expansion, so balance of risk must be assessed.
-
Antibiotics
- Culture blood, sputum, urine if pyrexial
- Treat established or clinically significant infection aggressively
- Consider prophylaxis for ICP bolts/EVDs and skull fractures (Ceftriaxone 1g IV od)
CPP Guidelines
-
If MAP inadequate to maintain CPP exclude and treat:
- · Hyovolaemia (including cerebral salt wasting and cranial diabetes insipidus)
- · Sepsis
- · Cardiac dysfunction (primary or neurogenic)
-
Then use inotropes/vasopressors as indicated to achieve MAP (usually noradrenaline +/- dobutamine)
Consider echocardiography +/- invasive cardiac output monitoring if:
- Acute or pre-existing cardiac disease
- Hypotension with high CVP
- Oliguria with high CVP
- Severe sepsis
- Pulmonary oedema
- Cardiac contusion
- High inotropic requirements, cardiac disease, over 50 years
Discuss with consultant: Patients with significant heart disease, acute lung injury, sepsis, failure to respond
ICP Guidelines
Exclude or manage:
- - Inadequate sedation (consider paralysis)
- - Inadequate ventilation or aggressive hyperventilation
- - Patient head positioning (30 degrees head up and head neutral)
- - Inadequate MAP (causing cerebral vasodilatation) or increasing MAP (in patients with loss of autoregulation may also cause cerebral dilatation)
- - Seizures (EEG may be required)
- - Pyrexia
- - Hypo/Hypervolaemia (or Hyponatraemia)
- - EVD Blocked? Discuss with neurosurgeons and consider withdrawing 5 mL aliquots
-
If ICP remains elevated > 20 mmHg (or dilated pupil) urgently repeat CT Head. If in doubt, discuss with Neurosurgeons
Prior to CT
- Temporary hyperventilation to maintain PaCO2 3.5- 4 kPa and
- Increase MAP by 10mmHg to maintain same flow through vasoconstricted cerebral vessels.
Management of raised ICP with Hypertonic Saline or Mannitol
- Only if Na <155 & Osmolality < 320 mosm/L).
- They both work by increasing plasma osmolality to ‘draw’ fluid from cerebral oedema, and also reduce blood viscosity to improve microcirculatory blood flow.
- Mannitol will usually cause a delayed diuresis.
- · 5% saline - 2mL/kg (e.g. 160 mL for 80kg patient) slow iv push centrally or via large vein 10mL 30% NaCl up to 60mL with water = 5%
- · 10% or 20% Mannitol – 0.25-0.5g/kg (IBW) (e.g. 100-200mL of 20% or 200-400mL of 10% for 80kg patient) over 15 mins.
-
After CT
- · Urgent D/W Neurosurgeons – Requirement for Surgery?
-
If ICP remains elevated and Neurosurgeons decide for Medical Management only:
- Increase sedation & paralyse (if not already)
- Aim for temp 36oC and consider lowering to 34-36oC in refractory cases.
- Consider Thiopentone bolus (3-5mg/kg); alternatively consider Ketamine bolus (1-2mg/kg) if BP tends to drop with sedation. Ketamine has been shown to reduce ICP, although a delayed increase may be seen.
- Consider boluses of lignocaine 1% over 5 mins (0.1 ml/kg) prior to suction/physio
Raised ICP despite ALL Medical Management above:
- Thiopentone coma – (BTF Guidelines 2016 Level IIB recommendation to control elevated ICP refractory to maximum medical treatment). See below – there is little evidence to recommend it & discuss with Consultant
- Decompressive craniectomy is not recommended by BTF (DECRA – More unfavourable outcomes, although lowers ICP and fewer ICU days, RESCUE-ICP – Identical (27%) patients in Medical management group with lower moderate disability or better. Decompressive Craniectomy resulted in fewer deaths but more patients with Upper severe disability (unable to leave home unassisted) or worse.
Large frontal-temporo-parietal DC is recommended if done - note 20% incidence of complications (including death) associated with subsequent cranioplasty.
Thiopentone coma
There is little evidence to support its use despite the theoretical advantages of a reduction in cerebral electrical activity, cerebral oxygen consumption, production of excitatory amino acids and lipid peroxidation. Although it may reduce ICP it can also reduce MAP.
A thiopentone bolus (3-5mg/kg) should be used as a therapeutic trial first, if there is no reduction in ICP (ensuring BP is maintained), continued infusion is not advised.
Cautions and contraindications:
- - Patient with hepatic or renal dysfunction
- - Elderly
- - Myasthenia
- -
Porphyria
|
Document Details |
|||
|
Title |
Traumatic Brain Injury |
||
|
Main points the document covers |
Management in Critical Care |
||
|
Who is the document aimed at? |
Critical Care staff |
||
|
Author |
Dr Tim Lowes |
||
|
Approval process |
|||
|
Approved by |
Critical care guidelines group |
||
|
Effective from |
Immediately |
||
|
Category |
Critical Care services JCUH |
||
|
Sub-category |
Neurosciences |
||
|
Review date |
)1/05/2022 |
||
|
Document Links |
|||
|
Required by CQC |
GPICS |
||
|
Required by NHSLA |
Yes |
||
|
Other |
|||
|
External references used |
|||
|
|||
|
Amendments History |
|||
|
No |
Date |
Amendment |
|
|
1 |
|||
|
2 |
|||
|
3 |
|||